
One of the focuses of my blog is STEM (Science, Technology, Engineering and Mathematics), and my most central principle is “Creating Ecosystems of Success”. While we tend to think of clinical medicine as strictly a ‘Healthcare Profession’, its foundations are rooted in the Basic Sciences. Medical Doctors/Physicians are likewise scientists who specialize in patient care and healing sicknesses.
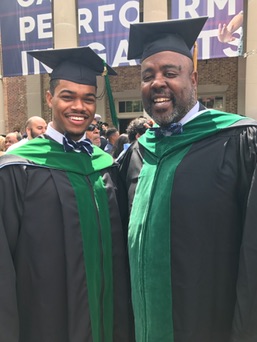
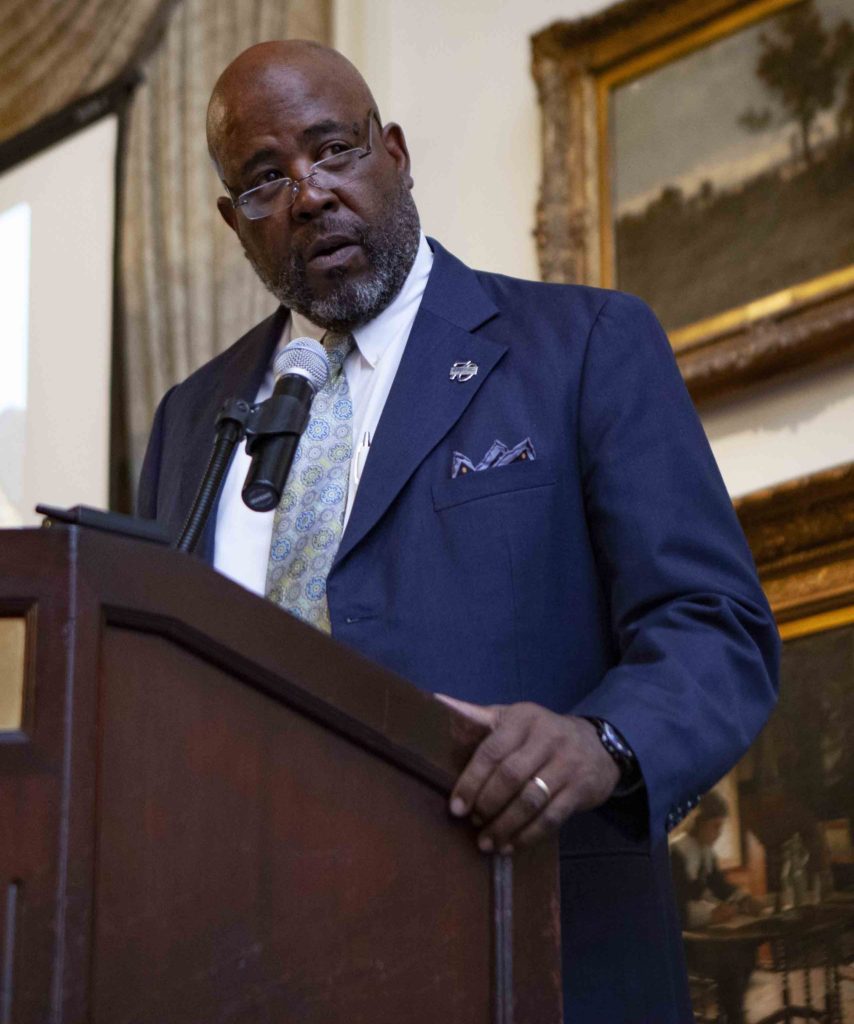
I recently met Dr. Cedric Bright in person through a mutual acquaintance at a family gathering. I’d heard of him through conversation, and I think I’d previously seen him before, as he was among the many physicians on Twitter using the ‘hashtag’ ‘#BlackMenInMedicine’. It turns out that Dr. Bright, the Associate Dean of Admissions at the East Carolina University School of Medicine , coincidentally knew Dr. Qiunn Capers, IV, whom I first saw using the hashtag.
At the gathering, Dr. Bright eagerly answered the questions of numerous medical school hopefuls who were in attendance. As they asked him questions, he in turn asked them questions about their preparation, their academic performance, standardized test scores, experiences in clinics and overall ambitions. At the recommendation of the host of the gathering, I listened in on Dr. Bright’s discussions and was fascinated by what he had to say.
With my blog having both education and a science focuses, and with me also knowing many medical school hopefuls, I seized the opportunity to ask Dr. Bright for an interview and he agreed. In the following interview with Dr. Cedric Bright, we discuss his background, his path into medical school and his career, and finally the current landscape of medical education – specifically what medical schools are looking for in prospects. I hope you enjoy the interview as much as I enjoyed doing it.
Anwar Dunbar: Thank you for the opportunity to interview you, Dr. Bright. Medical school has long been the destination for many undergraduates, and many people will love to hear what you have to say about what the journey towards practicing medicine entails. With that, can you talk briefly about yourself? Where are you from? What got you interested in medicine?
Cedric Bright: I’m originally from Winston-Salem, NC. I grew up there and attended a private boarding school. My parents were both public school teachers and believed in trying to give me and my brother every advantage we could have to be the best that we could be. They were of the ilk where, ‘This generation needs to do better than the last generation,’ and my parents made sacrifices for us so that we could go to private boarding schools.
From there I was accepted to Brown University for my undergraduate studies. I returned to attend medical school at the University of North Carolina at Chapel Hill (UNC). I did my ‘Residency’ back at Brown. I stayed on as faculty there for four years, and I wrote a paper which was published in the Journal of the National Medical Association, looking at perceived barriers in medical education by race and gender. That led to me being recruited to Duke University and the Durham VA-Medical Center. I spent 13 years there before I was recruited to come back to Carolina (UNC). I spent eight years at Carolina, and just left three weeks ago to come here to East Carolina.
AD: So, let’s go back to the beginning of your journey. Your parents – were they science teachers or were they teaching other subjects?
CB: They were general public school teachers. My father taught math and science in middle school, and my mother taught second grade in elementary school.
AD: What inspired you to become a medical doctor? Did you have a mentor in medicine? Also, are you the first medical doctor in your family?
CB: I’ll tell you that I’m not the first doctor in my family, but I also never met the person who was. He is a distant cousin on my grandmother’s side. I don’t recall hearing stories of him, though I’ve seen pictures. In terms of myself, my father being an educator brought home books for me and my brother to read. It was a series describing what doctors, nurses, engineers, fireman, police, etc., “do”. After reading those books, I decided that I wanted to be a doctor, and my brother wanted to be an engineer. Fast forward 20 years, he’s become an engineer. Fast forward 25 years, I’ve become a doctor.
AD: During your journey, were there any challenges in your undergraduate studies or throughout medical school itself? Or were you a ‘straight A’ student where the road was all set for you?
CB: I was nowhere near a straight A student, but I was a hard worker. My parents put me in some courses that taught me how to study. In doing so, they helped me with my concentration. I probably would’ve been diagnosed as “Attention Deficit Disorder” (ADHD). I still have lot of ADHD tendencies now in my old life.
I learned techniques on how to manage my thoughts, my ability to focus, and even with that I had some academic difficulties. I learned how to use the system – how to ask for help – how to not be afraid to admit that I didn’t know something. I learned how to visit teachers during their office hours, and how to spend time after class working on things. I learned how to ask my colleagues who were willing to help – all those types of things.
I did reasonably well in high school. I particularly did well in Chemistry; my teacher was my football coach. I was quite fond of him and he helped me understand Chemistry very well, such that I did very well in it in college.
I did quite well my freshman year in college. Subsequently, I had the ‘sophomore slump’. I pledged a fraternity the spring semester of my freshman year, and I came back and ‘acted’ that fraternity the first semester of my sophomore year, and my grades summarily crashed. At that same point in time, I decided that I didn’t like Biology anymore and I didn’t want to do Chemistry. I decided that there must be something else that I could major in. Low and behold I’d taken some courses in Film because I’d been interested in it, and so I decided that I’d major in it.
AD: Oh, interesting.
CB: My Pre-Med Advisor said, ‘You don’t have to major in a science to go to medical school,’ and I said, ‘Okay, I’m going to take you at your word on that!’ So, I ended up majoring in Film (Semiotics), and what it taught me was how to understand non-verbal communication, understanding how the body moves and when a person’s body is or isn’t reflective of their verbal statements. Being able to interpret my patients better, I think that helped me in the long-term.
AD: Interesting.
CB: So, I pulled my grades up my next two years after my sophomore year, and I think that’s why I got into medical school. My grade point average (GPA) wasn’t great – it was less than a 3.0 and I’ll leave it at that. I had to take the Medical College Admissions Test (MCAT) three times to get a score that would at least get me noticed. I think the final score that I got was a 27. I only applied to two medical schools and I got into the UNC, which was crazy.
After getting in, I was advised to do a summer program and I’m grateful that I was. It surrounded me with like-minded individuals. The first thing I tell young people today is to make sure you do some type of summer program to surround yourself with other like-minded individuals. They become your colleagues of the future.
AD: Interesting.
CB: The program also helped me to understand the difference between undergraduate-level and graduate-level studying. Had I not done the program, I’m sure that I would’ve had more academic difficulty during my first year.
AD: So, you’re referring to the complexity of thought and….
CB: And the amount of time you must put into it. For instance, I was used to studying maybe an hour or two a day, and then ‘cramming’ towards the end and still being able to get a good grade. You can’t do that in medical school. In medical school you must put in four to five hours every day. You must put in six to eight hours on the weekend – it’s a ‘grind’ and you must get used to that grind. You have to become disciplined and not fall prey to the ‘Jedi-Mind Tricks’ that your classmates would throw on you by saying that they spent the whole weekend hiking the Appalachians. They might have hiked a mile, but they spent the rest of the time studying. They want you to think they didn’t. So learn not to fall for the Jedi-Mind Tricks. Everyone is working hard in medical school.
AD: Jedi-Mind Tricks (laughing). What was your ‘specialty’?
CB: My specialty ended up being ‘Internal Medicine’, but that’s another story.
AD: Okay.
CB: Let me finish this point. I prayed before I got into medical school. I said, ‘Lord, don’t let get into medical school if I’m not going to graduate!’ So, when I got in, that took a load off me because I knew that I’d prayed and that he’d answered my prayers and I knew that I would graduate. The question then became how. I’d done the summer program, but my first semester of medical school, seemingly on every test I was one to two points above passing and I wasn’t ‘killing’ it by any means.
I was the last man on the totem pole probably every time and on every test. At the end of my first semester, I passed three of my courses, but I failed one by less than a half a point. So, I ended up having to remediate that course during the summer, but after coming back from the Christmas break, I realized that I couldn’t do the same work that I’d been doing and working the same way. I had to change my study habits.
For the most part, I’d studied with one of my frat brothers. It worked well, but it didn’t work well enough. So I said let me branch out and see if I can study with some other people. So I started studying with some other people who didn’t look like me and I started finding ways in which they studied that reminded me of the study programs my father had put me in back in the day. I started re-utilizing those study techniques and suddenly, I began to thrive. I had to make an adjustment and go back to a study technique that really helped me out when I was younger, and it turned out to be the elixir that I needed in medical school.
From that point on in my second year, I moved into a house with six to seven other medical students. Each night we’d study until about 10 to 10:30 at night and we’d come out to the common area of this house and have this massive ‘Quiz Bowl’. The whole point of the Quiz Bowl was for me to take the most esoteric fact that I knew and try to stump them, and for them to take the most esoteric fact that they knew and try to stump me.
Now here’s the key Dr. Dunbar. If I stumped them, I had to teach them. And if they stumped me, they had to teach me. The effect of that was that by the time we got to the exam, we’d asked so many questions of each other from so many different perspectives that there weren’t too many questions on the exam that we hadn’t already discussed. So like a ‘rising tide’, we all did very well. What that speaks to is how you work in medical school to get the ‘volume’. It’s not aptitude that impedes people’s progress in medical school, it’s dealing with the volume.
It’s kind of like trying to eat an elephant. If you’ve got one person trying to eat an elephant, it takes a long time to do it. But if you’ve got seven to eight people trying to eat the elephant with everyone describing what they’re biting and how it tastes, the texture of it, you get to know the whole elephant, but you just ate a part of it. Does that make sense to you, sir?
AD: Yes.
CB: So that’s one of the most valuable lessons I’ve ever learned about approaching large volumes of work. If you approached it first being responsible for taking care of your own individual preparation and coming together and working with other individuals who have put in their own individual preparation, you can work very effectively as a group. But it first starts with individual preparation.
AD: Okay, so there’s a component there that requires individual preparation and then there’s a teamwork component there.
CB: That’s correct. The individual preparation gets you to 50%, but that team component gets you to 90%.
AD: That makes sense. When I first got to graduate school, I was used to working by myself, and I discovered that I couldn’t do that and get the grades that I needed. Just quickly, which fraternity did you pledge?
CB: I pledged Omega Psi Phi.
AD: In term of my next question, you discussed this at the gathering where we met, and it really resonated with me. When I was an undergraduate student at Johnson C. Smith University in the late-1990s, many of us pondered practicing medicine, but few of us thoroughly understood what it took to get into medical school. Aside from the academic credentials, what are some of the personal qualities aspiring medical students need to be successful and, in general, what are you all looking for? I remember you saying that you want them to have touched patients before.
CB: That’s true. We want to see that you’ve had a journey of learning about the didactics and the science component, yes, but also about the humanity – doing volunteer service for people less fortunate than yourself. This helps you to understand the social determinants and sometimes the behavioral determinants of health, and how they manifest themselves in our community.
We want you to have spent some time doing some type of hands on patient care, whether its learning how to take blood pressure, learning how to take vital signs in the doctor’s office, or being an Emergency Medical Technician (EMT), and helping to triage patients and get them to the emergency room. Or it could be just driving an ambulance to take people to their regular hospital visits, being a nurse, or being a Certified Nursing Assistant (CNA) doing the hands-on dirty work in the hospital. Lastly, it could be being a pharmacy tech spending time working in a pharmacy where people are coming in asking questions about their medications. And helping them understand the side effects, and reactions from other drugs and things of that nature or being a hospice volunteer to helping people with end of life issues.
These are the types of things we’re looking for hands-on wise. There are a lot of smart people in the world, but there’s a difference between being smart and having intelligence. We’re looking for more intelligent people than we are smart people. Smart people know how to answer questions. They can get a question right all the time, but they don’t know how to talk to people. They don’t know how to deal with the ‘human component’. Intelligence is knowing what you know and being able to apply it to the people in front of you at the right time, for the right person, for the right reasons.
AD: Now in that same vein, if I recall correctly, in terms of determining why students want to attend medical school, you’re not looking for canned, ‘cookie cutter’ answers. You want to hear some depth to their answers, right?
CB: Yes. The ‘depth’ comes in multiple ways. For example, when someone writes about their experiences, I don’t care so much about what they did, I want to know how it made them feel. I want them to be able to share with me if there was a significance that changed their view of death if they worked in a hospice; how they think the healthcare system works as the ‘donut hole’ as it goes to prescription drugs.
I want them to be able to share if they know the significance of how nurses are so overworked and have too many patients, such that a CNA becomes so very important; how to take care of people in the hospital, or how to take care of people in the clinic as a medical assistant. Why (what was your motivation)? What did you feel? What did you observe? What did you learn? That’s more important to me than what you did.
AD: So, this is my last question. The landscape of medical education and medical school, has it changed since you were a student yourself? We have a lot of technology now. People communicate differently. I’m sure the actual medical approaches have changed. Can you talk about how things have changed from then to now?
CB: I think when I was coming through, we didn’t have as many imaging tests and diagnostic procedures, so our touch to the patient became more important. Doing the appropriate physical exam was enough for you to come to a diagnosis. You didn’t have to have an X-ray. You didn’t have to have a ‘CT’, because if you did your exam right, you knew what your exam told you. Now we depend too much on technology to tell us what’s wrong with a person, and it doesn’t always equate to us finding the right answers on how to take care of people.
I also think that our technology and having to ‘keyboard’ so much on these electronic records takes us away from the human touch – the humanity of medicine which is the one-on-one conversation with our patients because we’re too busy ‘charting’. Our eyes don’t meet enough. Patients wait months to come see a doctor, not watch a doctor type. Seeing a doctor means we have eye-to-eye contact and we talk as two human beings intimately in one setting, and I think that’s becoming a lost art in medicine. Doctors are under time crunches to see more patients and to make the same amount of money, or to make more money.

AD: I think that rolls into my last two questions. I know that every student is different, but on average, what are the major learning points for the medical students when they come in, because I imagine that these are all very bright individuals. What are the main things they must learn? Is it what you described for yourself? Or is it something else?
CB: I think the main thing they need to learn is that it’s not their aptitude that’s going to determine their altitude, it’s their attitude. If they come in with the right attitude of wanting to learn, and sacrifice whatever it takes to learn, and not come in with the attitude of, ‘I’m not doing this or, I’m not doing that’. That just doesn’t work in medicine. They also must learn how to deal with failure. The thing about medicine as with all walks of life, Dr. Dunbar, is that we all fall down. There’s no shame in falling down and we shouldn’t fall apart the first time we fail.
But what we should do is learn from the mistakes that we’ve made. Learn from what has occurred, grow and move forward, and get back up. I like to say that there’s no shame in falling down. There is shame in laying there. And don’t let anybody fool you into thinking that their life is perfect. All that is, is a mask. We all fall down. We all have imperfections. We all fall short of the glory.
AD: My high school basketball coach used to tell us that exact same thing about attitude and altitude. My last question is going to be a little more global. Under the Obama Administration, we had the Affordable Care Act (ACA), and now that’s kind of been stripped down. In terms of the medical field itself, do we still have enough doctors? Is it still a thriving field?
CB: It’s very much a thriving field, and there will always be a need for doctors. I wholeheartedly believe in that. Artificial Intelligence will never be able to replace doctors, because they don’t have the touch. There’s more than enough need for physicians and, in many places, we’ve said there’s going to be a shortage of physicians in the future. That’s because we have areas where more physicians are passing away than physicians are being made.
The ‘Baby Boomers’ are probably a third of our physicians that we have in the workforce and they’re retiring at a rate of almost 1,000 every month. So, we’re going into a crisis of having more physicians retiring than those who are graduating. It’s a very interesting dichotomy and the American Association of Medical Colleges has been preparing different reports to show that. I was actually looking at one the other day.
The bottom line is that there’s a two-fold problem. We’re not making enough doctors and doctors are retiring, or we have enough doctors and there’s a maldistribution of doctors. Some would argue that theory. We have enough doctors, but all of our doctors want to practice where there are other doctors. But in actuality, we may need to redistribute them so that they practice in other areas that are rural and have less physicians in that area.
AD: Well, Dr. Bright that’s all the questions that I have. Thank you for your time and for sharing your path and knowledge and expertise about the medical field. A lot of people will benefit from this, and I look forward to doing it again.
Thank you for taking the time to read this interview. If you enjoyed it, you might also enjoy:
• Dr. Quinn Capers IV discusses Implicit Bias and the #DropAndGiveMe20 campaign
• Dr. Quinn Capers, IV discusses his path, #BlackMenInMedicine, and the present landscape of medical education
• The story of how I earned my STEM degree as a minority
• How my HBCU led me to my STEM career
• Researching your career revisited: Wisdom from a STEM professor at my HBCU
The Big Words LLC Newsletter
For the next phase of my writing journey, I’m starting a monthly newsletter for my writing and video content creation company, the Big Words LLC. In it, I plan to share inspirational words, pieces from this blog and my first blog, and select videos from my four YouTube channels. Finally, I will share updates for my book project The Engineers: A Western New York Basketball Story. Your personal information and privacy will be protected. Click this link and register using the sign-up button at the bottom of the announcement. If there is some issue signing up using the link provided, you can also email me at bwllcnl@gmail.com . Best Regards.
 One of the focuses of my blog is STEM (Science, Technology, Engineering and Mathematics), and my most central
One of the focuses of my blog is STEM (Science, Technology, Engineering and Mathematics), and my most central  QC: I attended public schools in Dayton, Ohio on the city’s west side – the ‘black’ side of town. I was always enamored with
QC: I attended public schools in Dayton, Ohio on the city’s west side – the ‘black’ side of town. I was always enamored with  QC: After spending the first eight years of my career in a private
QC: After spending the first eight years of my career in a private  QC: Very little that has been openly stated, but we are sensitive to the fact that there are likely some who feel it’s divisive and not promoting unity. We think that it’s possible to promote Black men in medicine while supporting many other groups. Many of us also tweet using other hashtags that preceded #BlackMenInMedicine, such as #WomenInMedicine, #ILookLikeASurgeon (which promotes images of women in surgery), and others. We took this on because the low numbers of Black men in medicine, in academic medicine, in leadership roles, and amongst medical school applicants has reached a crisis. I should also point out that we, the original creators of this campaign, do not feel that use of the hashtag is proprietary. Anyone who wants to promote diversity in medicine, and particularly encourage Black men to pursue medicine, is welcome to use the hashtag. In fact, we encourage it.
QC: Very little that has been openly stated, but we are sensitive to the fact that there are likely some who feel it’s divisive and not promoting unity. We think that it’s possible to promote Black men in medicine while supporting many other groups. Many of us also tweet using other hashtags that preceded #BlackMenInMedicine, such as #WomenInMedicine, #ILookLikeASurgeon (which promotes images of women in surgery), and others. We took this on because the low numbers of Black men in medicine, in academic medicine, in leadership roles, and amongst medical school applicants has reached a crisis. I should also point out that we, the original creators of this campaign, do not feel that use of the hashtag is proprietary. Anyone who wants to promote diversity in medicine, and particularly encourage Black men to pursue medicine, is welcome to use the hashtag. In fact, we encourage it. QC: I applied to
QC: I applied to